SHARE
Rheumatoid arthritis is a common cause of bone loss and osteoporosis. Being a chronic inflammatory disease, Rheumatoid Arthritis affects the articular cartilage but can cause bone destruction and, eventually, bone loss. However, Rheumatoid Arthritis is a systemic disease that can affect the joints and other organs in the body (e.g, lungs, heart, eyes, kidneys).
In this article, we will discuss
- How Rheumatoid Arthritis affects your bones?
- What are the risk factors for bone loss?
- How do we diagnose bone loss?
- What are the consequences of bone loss?
- How do we treat bone loss?
How Rheumatoid arthritis affects the bones?
Rheumatoid Arthritis affects the bones and may cause osteopenia and osteoporosis. Osteopenia is a condition in which bone loss causes the weakening of the bones. Osteoporosis is a more advanced bone disease that can lead to easy fractures.
What are the risk factors for osteoporosis in patients with Rheumatoid arthritis?
Osteopenia and osteoporosis tend to happen more often in certain patients with Rheumatoid Arthritis.
Here are the most important risk factors:
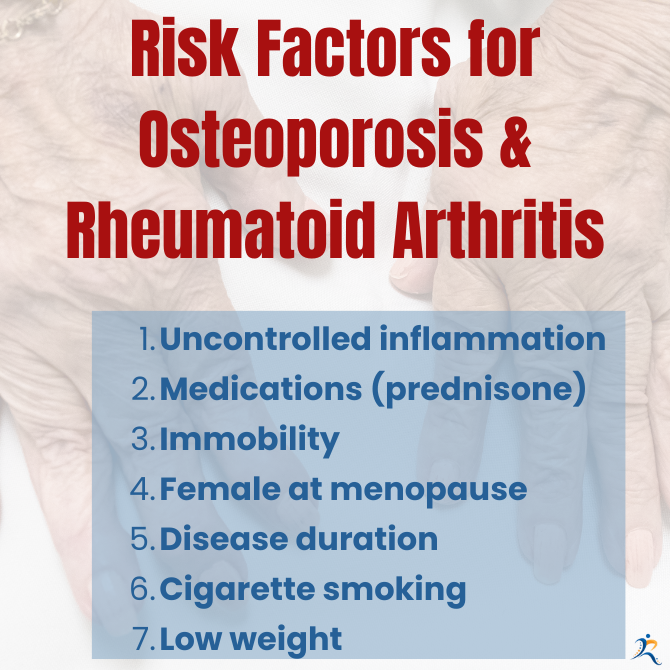
- Ongoing, uncontrolled inflammation from Rheumatoid Arthritis
- Medications (e.g, steroids like prednisone in high doses or used for a prolonged time)
- Immobility for long periods. That is why exercise is essential in treating Rheumatoid Arthritis patients, as it will induce less bone destruction and more new bone formation.
- Female at menopause – a reduction in estrogen hormones caused by menopause is an individual cause of osteoporosis.
- Disease duration – the longer the disease, the higher the risk of osteoporosis.
- Cigarette smoking
- Low weight. Interestingly, a lower weight may be associated with an increased risk of osteoporosis.
How do we diagnose bone loss in Rheumatoid Arthritis?
Osteopenia and osteoporosis are diagnosed by using a dual-energy x-ray absorptiometry (DEXA) scan. Since every patient with Rheumatoid Arthritis is at risk for osteoporosis, a DEXA scan should be done every two years in patients at risk.
What are the consequences of bone loss in patients with Rheumatoid Arthritis?
Patients with Rheumatoid Arthritis have around 60 to 100% risk of osteoporotic fractures compared to patients who do not have Rheumatoid Arthritis. In one study in the United Kingdom, the prevalence of osteoporosis in patients with established Rheumatoid Arthritis referred for a bone mineral density (BMD) study was approximately 1.5- to 2-fold greater than age- and sex-matched patients without Rheumatoid Arthritis]. Hip fractures are more likely to happen in persons with Rheumatoid Arthritis. Immobilization from a fracture can exacerbate bone loss and lead to faster onset of osteoporosis.
Osteopenia can affect the small joints attacked by inflammation and can eventually lead to joint erosions.
How do we treat bone loss and osteoporosis in Rheumatoid arthritis?
First, it is recommended to obtain a DEX scan to evaluate the degree of bone loss. Second, we use a risk assessment tool called Fracture Risk Assessment Tool (FRAX) to consider many of the patient’s risk factors and estimate the risk for long-term fractures. If the risk for fracture is high, then treatment is recommended.
Lifestyle changes
Patients with Rheumatoid Arthritis should always consider extremely valuable lifestyle interventions. Those changes include decreasing or, even better, stopping alcohol intake, giving up smoking, and trying to maintain an active lifestyle. Exercises are strongly recommended, as they have been proven to reduce bone loss. Exercise such as walking, climbing stairs, and dancing. Also, resistance exercises, such as lifting weights, can help strengthen the bones.
Moreover, an adequate intake of Calcium of around 1000–1200 mg together with Vitamin D3 supplementation (800 UI/day) has been shown to reduce the risk of falling by 20% and reduce the risk of subsequent fracture risk.
Medications
Bisphosphonates (e.g. alendronate/Fosamax, risedronate)-are the most widely used medication in osteoporosis. They have been shown to reduce the risk of vertebral fractures in patients with Rheumatoid Arthritis.
Teriparatide and Denosumab. Teriparatide is a parathormone analog that increases bone formation. Several studies have shown that Teriparatide compared with the drug alendronate, resulted in significant vertebral fracture reduction.
Denosumab is a human monoclonal antibody, and it was found that compared with Risendronate, it had better outcomes on spine and hip osteoporosis.
Conclusion
As mentioned, osteopenia and osteoporosis can have devastating consequences, from increased risk of fracture to disability, and even be the cause of death. We encourage all patients with Rheumatoid Arthritis to get the disease under good control, to continue with exercise, and adopt a healthy lifestyle without alcohol and smoking. Talk to your doctor about your risks of developing osteoporosis and get a DEX scan when needed. At times, medications are needed to help strengthen your bones.
This is an educational article that aims to broaden your knowledge, but it does not offer you medical advice. If you have an autoimmune disease, like rheumatoid, and need help, you are welcome to check out our practice and get the help you need when you need it the most. Rheumatologist OnCall is a telemedicine rheumatology practice that broadens access to a specialist in a very short time, when you need it the most and breaks geographical barriers. Check out the states where we are licensed to see patients in the US and reach out to us if needed. We are happy to serve you.